Anna hasn’t always been a benefits expert—life turned her into one. As the mother of a son with Autism, she understands the complexities of the confusing web of institutions, documentation, and convoluted terminology surrounding the Georgia Medicaid waiver programs. Like many of us, she turned to the internet for answers and tried to connect with others who had walked the same path. But nothing provided the clarity she needed. At that time, everything seemed shrouded in mystery.
Determined to find a better way, Anna developed her own approach to secure a bright future for her son, who is now in his 30s and thriving. From Anna’s knowledge and experiences, Bobby Dodd Institute (BDI) Benefits Navigation program was born. Today, Anna Maki is the Director of Program Services at BDI, where her mission is to help individuals with disabilities obtain the services they need to ensure a positive future for their children.
BDI’s Benefits Navigation team has guided numerous families, like the Park Family, through the process and helped them obtain waivers. Their long journey began when Will was born with a rare genetic disorder. He lives with multiple disabilities. His family sought help from the public school system, but they found they needed additional support as Will approached adulthood. Filled with uncertainty about Will’s future, the Park Family turned to Bobby Dodd Institute. BDI’s Benefits Navigation team guided Will’s family through the process of applying for Supplemental Security Income (SSI) when Will turned 18. Together, the Benefits Navigation team and the Parks developed a futures plan for Will and secured approval for a Medicaid waiver—a major win, after being on a waiting list for 10 years.
In 2023-2024, the Benefits Navigation team secured 38 waivers.
Through working with individuals like Will, BDI has developed a unique process that we are now sharing in the following paragraphs. In this blog post, you will find essential guidance to help you understand the Georgia Medicaid waivers, learn about the likelihood of receiving benefits, explore the application process, and gain an understanding of the ways to identify the most suitable services for your specific needs.
What is a Waiver?
Simply put, the Georgia Medicaid Waiver helps people with disabilities or elderly individuals live in their homes or communities while receiving the services they need, rather than being placed in an institution. Individuals must meet institutional level of care (level II) to be eligible for services.
“What we’re establishing,” Anna explained, “is that the individual meets the level of care required for an institutional setting, but we don’t want those services provided there. We don’t want our loved ones in a nursing home—we want them in the community.”
Before 1999, people with intellectual and developmental disabilities were often sent to institutions for care, instead of staying in their family homes. However, a Supreme Court decision on June 22, 1999, changed everything for millions of Americans and their families. The Court ruled in Olmstead that just because people need assistance with daily living, it doesn’t mean they should be unnecessarily institutionalized.
Before we dive deeper, one of the first things you need to know before starting the process is that you must be very diligent with your documentation. Gather all documentation of the individual’s condition and be prepared to demonstrate that they meet the institutional level of care. “What that’s really asking is: can this individual live independently? If the answer is no because they need help with activities of daily living or emotional self-regulation, then they’re more likely to meet the Level II care requirements,” Anna added.
Understanding Georgia’s Waiver Programs
In Georgia, there are several different waiver programs, all of which fall under the umbrella of home and community-based waivers.
- Georgia Pediatric Program
- Community Care Service Program
- Elderly and Disabled Waiver
- Independent Care Waiver Program
- NOW/COMP
- New Options Waiver
- Comprehensive Waiver
The Georgia Pediatric Program is designed for minors with significant care needs including significant behavioral needs, but you can remain in the program beyond age 18. The recent trends are showing that the Department of Behavioral Health and Developmental Disabilities (DBHDD) encourages individuals to maximize services through Family Support Services and the Georgia Pediatric Program before receiving a NOW/COMP waiver.
The Independent Care Waiver Program is similar to the NOW/COMP waiver in terms of funding and services. Individuals receiving this waiver can get help at home with daily activities, like getting ready in the morning and going out into the community. This waiver is usually for those with physical impairments rather than cognitive disabilities. It typically covers tasks like transferring from bed to a wheelchair, bathing, and personal care, but unlike NOW/COMP, it does not cover 24-hour care or group homes. Often, individuals with a traumatic brain injury receive services through the Independent Care Waiver rather than NOW/COMP.
The Elderly and Disabled Waiver is for those who need care less frequently—perhaps only one or two days a week—rather than every day. Programs like SOURCE and Meals on Wheels may also be connected to this waiver.
The Community Care Services Program (CCSP) offers some flexibility but is generally not a long-term solution for individuals with intellectual and developmental disabilities. Occasionally, it may be used for short-term care. The risk with CCSP is that if you are receiving services under this program and you’re still on the planning list for NOW/COMP, it may be hard to show that you’re most in need of a NOW/COMP waiver.
That is why you need to be strategic when applying for waivers and ensure that you choose a program that best fits your needs. “For most individuals under 21, the focus is on the Georgia Pediatric Program. Once they’ve aged out, the primary options are usually the NOW/COMP waiver or the Independent Care Waiver. I generally recommend reserving the Community Care Services Program and the Elderly and Disabled Waiver for individuals who may not meet the eligibility criteria for NOW/COMP,” Anna says.
What Are NOW/COMP Waivers
The NOW/COMP waiver offers a full range of services specifically for individuals with intellectual and developmental disabilities. These waivers are generally awarded after individuals age out of the school system, typically at age 22. This program is managed by DBHDD.
Currently, there are over 7,000 people on the planning list for a waiver, but DBHDD has not released specific details, such as the ages of those on the list. “I think that’s really important information to know for us to be able to allocate appropriate resources. And this is a little disappointing because we’ve had back-to-back years where the state has approved more than 500 waivers. If we keep going on that pathway, then we’re going to whittle down these 7,000 waivers pretty soon. Unfortunately, with this fiscal year that started July 1, only 100 awards were budgeted,” explained Anna Maki. It is also important to note that it’s not a numbered list; you’re either on it or not, and you’re either considered “most in need” or not.
The NOW/COMP waivers are funded through a combination of state and federal dollars. If Georgia had expanded Medicaid, this wouldn’t be a problem. How this process actually works? DBHDD proposes a budget to the state, and the governor’s office allocates a certain number of waivers each year. There’s significant advocacy behind the scenes, but ultimately, the final budget determines the number of waivers. This fiscal year, the Georgia Council on Developmental Disabilities proposed 2,400 waivers, as the state had a budget surplus. Despite this, only 100 waivers were approved. “This is disappointing because more people will be added to the planning list or be diagnosed with an eligible condition throughout the year. The math isn’t working in our favor right now, but we hope to continue our advocacy efforts. It’s important to advocate with your legislators to help them understand the importance of this program,” urged Anna.
Eligibility Criteria for NOW/COMP Waivers
To be eligible for a NOW/COMP waiver, the individual must have a diagnosed developmental disability. Developmental disability is defined as a chronic condition before the age of 22, which may involve cognitive and/or physical limitations.
DBHDD considers conditions like Autism and Cerebral Palsy as closely related to intellectual disabilities. For individuals with Autism, they focus on cognitive function, particularly full-scale IQ, as well as adaptive function which indicates abilities with day-to-day activities like functioning in the home/community. Even if an individual’s full-scale IQ is above 70, they may still qualify for a NOW/COMP waiver depending on their adaptive function scores. Both cognitive and adaptive functions are critical in determining eligibility. The adaptive function assessment, like the Vineland Adaptive Behavior Scale, is essential. It includes three domains, and DBHDD prefers to see all three domains with scores below 70. This requirement can sometimes be tricky, but it is an important trend in determining eligibility.
How to Apply for a NOW/COMP Waiver
The NOW/COMP application is deceptively simple, consisting of two pages. The first page requests basic information like the individual’s name, address, gender, legal status, and the referring party’s contact information. Legal guardianship is also covered—if someone has not gone to court to establish guardianship, the individual is considered legally competent. The second page asks what services are needed, but it is a general question about helping the individual live independently in the community. The key part of the application is the supporting documentation, particularly the psychological evaluation. It’s crucial to ensure that the evaluation includes both cognitive and adaptive function scores.
The application is then followed by a “scavenger hunt” for necessary documents, including a psychological evaluation, proof of citizenship, and Social Security benefits documentation. It’s important to note that you can get on the planning list without Medicaid, though you cannot be awarded a waiver without Medicaid, as this is a Medicaid waiver. However, there are many classifications of Medicaid in Georgia, and one is tied specifically to NOW/COMP.
Another misconception is that guardianship is required, which is not the case. If you have guardianship, you’ll need to provide the guardianship letter, but it’s not necessary to apply for the waiver. You will need basic documents like a Social Security card and a psychological evaluation (psych eval). The Individualized Education Program (IEP) might also be requested, but it often highlights strengths, which may sometimes confuse the evaluation of the individual’s true needs.
To apply, you submit the application and all supporting documents to your regional DBHDD office either by mail or via the DBHDD online portal. Georgia is divided into six regions, and the application includes a list of counties to help identify where to send the application. Once your file is complete, an intake evaluation is scheduled. This is mostly a way for officials to ensure that what’s on paper matches the person’s actual needs. Families should avoid overstating the individual’s abilities, as this may reduce the perceived need for the waiver.
After the intake, if it’s determined the individual needs support, a letter will confirm that the person is pre-determined eligible and on the planning list. It’s essential to build a relationship with the planning list navigator and clearly communicate the level of support the individual requires. The navigator conducts an annual determination of need assessment, evaluating support needs for daily living, community access, and health risks, which helps prioritize who is most in need. “If you don’t know your navigator,” Anna says, “it’s unlikely you’ll get a waiver soon. It’s crucial to keep the navigator informed of significant changes, such as new diagnoses or changes in behavior, which may increase the individual’s placement on the list. Reporting these changes is more effective than frequently asking for updates on your status.” Navigators also want to see that you’re using all available resources, like Family Support services. If you aren’t using them, it may reduce your priority on the list. Additionally, if a caregiver passes away, this can significantly increase the individual’s need for support. Similarly, behavioral issues that could involve law enforcement also increase priority.
“The waiver system can feel reactive, focusing on current needs rather than planning for future ones. The DBHDD is concerned with immediate needs, not future concerns, so it’s vital to emphasize present challenges when advocating for a waiver. Navigators, while seemingly stoic, tend to be kind and supportive. The goal is to show that the individual needs support. After the navigator makes a recommendation, the supervisor makes a final decision,” Anna explained.
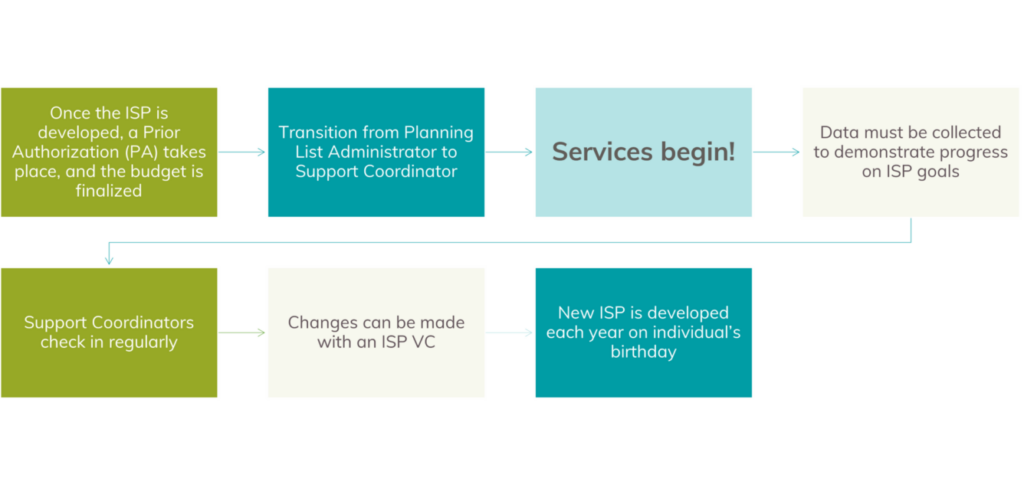
If approved, you move from a navigator to a planning list administrator, who helps set up the waiver process. You’ll need to select a fiscal agent to handle the funding, as the money doesn’t come directly to you. You’ll also choose a support coordinator who develops an Individual Support Plan (ISP) and checks in on progress throughout the year. Several assessments—Supports Intensity Scale, Health Risk Screening, and Behavioral Assessment—are conducted to determine the specific services needed, which then determine the budget.
Once the ISP is in place, with all goals and services defined, services can start. Individuals receive support coordination and fiscal management services. Support coordinators usually check in quarterly, or monthly in more intensive cases. If you choose to self-direct, you have more control over staff hiring and payment but take on more responsibility for documentation.
Additional services are based on the individual’s needs, not wants. It’s important to focus on those needs when advocating with DBHDD. The most common services include:
- Support Coordination/Fiscal Management
- Community Access Group (day program)/Community Access Individual
- Prevocational Support
- Community Living Supports (services in individual’s own home)
- Community Residential Alternative (group home or host home – COMP)
- Respite (max 30 days)
- Behavioral Support
- Supported Employment
Community access can be provided in a group setting like day programs or individually, which may include one-on-one support for activities like going to the gym or grocery shopping. Pre-vocational support and supported employment are also available and are often initiated through Georgia Vocational Rehabilitation Agency (GVRA).
Community living supports involve assistance in the individual’s home, like help with medication management, meal preparation, laundry, and safety. Some individuals also require companion assistance. For those who cannot live alone, community residential alternative services, think group homes or host homes, are available through the COMP waiver.
It’s important to distinguish between live-in care and 24/7 care. Live-in care provides supervision but doesn’t require staff to be awake around the clock, while true 24/7 care involves continuous duties performed by staff. This distinction is crucial when making requests.
Additional services include up to 30 units or days of respite care and behavioral support, which can involve developing a behavior intervention plan or supporting social skill development. The services provided are always based on the documented needs of the individual.
If circumstances change (Ex. if you want to explore a group home or host home), the support coordinator will update the ISP. Once you have a waiver, adding or changing services is easier than obtaining the initial waiver. The ISP is updated annually, based on the individual’s birthday, and the services continue as needed.
How to Apply for a NOW/COMP Waiver—Simplified Checklist
NOW/COMP application includes:
- List of required documents to attach to application.
- Identification information
- Contact information.
- Guardianship
- Requested services.
Steps
- Submit application and supportive documentation to regional DBHDD office Intake Coordinator
- Within 30 days of a complete application, Intake Evaluation is scheduled.
- Once determined eligible, DBHDD provides a letter.
- Individual is placed on a Planning List
- Planning List Navigator is assigned.
- Conducts Determination of Need assessment to identify key service needs. Assesses who is “most in need” and makes recommendations of awards. Remember, you can use Family Support Services to demonstrate you are utilizing all available resources.
Next steps
- Case is transferred to a Planning List Administrator
- Select Fiscal Agent
- Select Support Coordinating Agency
- Complete Assessments
- Support Intensity Scale
- Health Risk Screening Tool
- Behavioral Assessment
- Complete Self-Direct training
- Identify Providers
- Develop an Individual Support Plan
Obtaining a waiver can be a tiresome and frustrating process, but following these steps can help you alleviate the pressure. If you need additional help and personalized advice, email empowers@bobbydodd.org or apply for services directly.